Starting September 1, 2025, ADULT Medicaid recipients age 21 and over who are newly applying for Personal care services ["PCS"], Consumer-Directed Personal Assistance (CDPAP), or Managed Long Term Care (MLTC) or Medicaid Advantage Plus (MAP) enrollment must meet a higher eligibility test to qualify. This is called the "Minimum Needs" test or the "Three-ADL Test" or ADL Thresholds." This restriction on eligibility was enacted by NYS in 2020 but was on hold until Sept. 2025 because of Maintenance of Effort Requirements under the federal ARPA COVID relief law. See more here.
View recording here of NYLAG webinar presented on Aug. 26, 2025 and download Powerpoint presentation here.
IN THIS ARTICLE--
-
What are the new ADL Thresholds? - Which ADLs count and How Much Assistance With the ADL Must be Needed?
-
The 3-day "Lookback" - Only ADLs for which Assistance Provided in the 3 Days before the assessment count.
-
-
Fair Hearing & Other Strategies if DENIED MLTC or Home Care Based on the ADL test
-
CMS Approval of the ADL Thresholds and NYS Senate Bill to REpeal
What are the New Minimum ADL Thresholds?
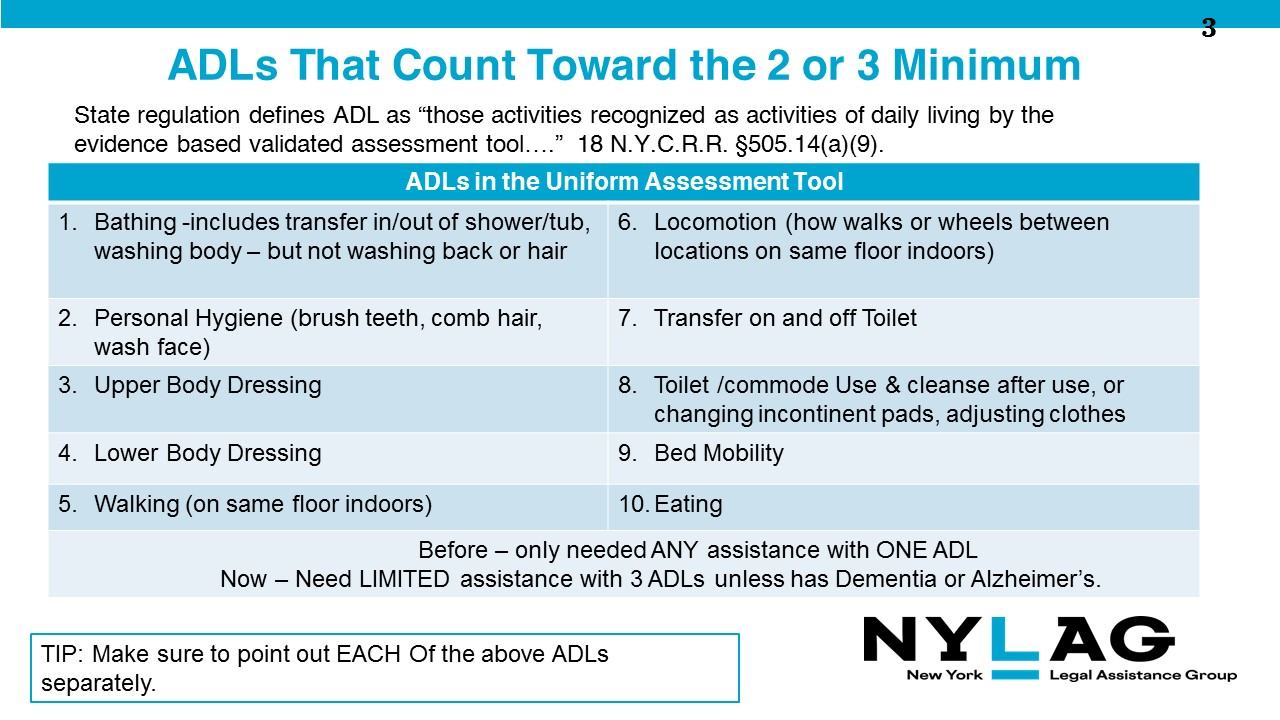
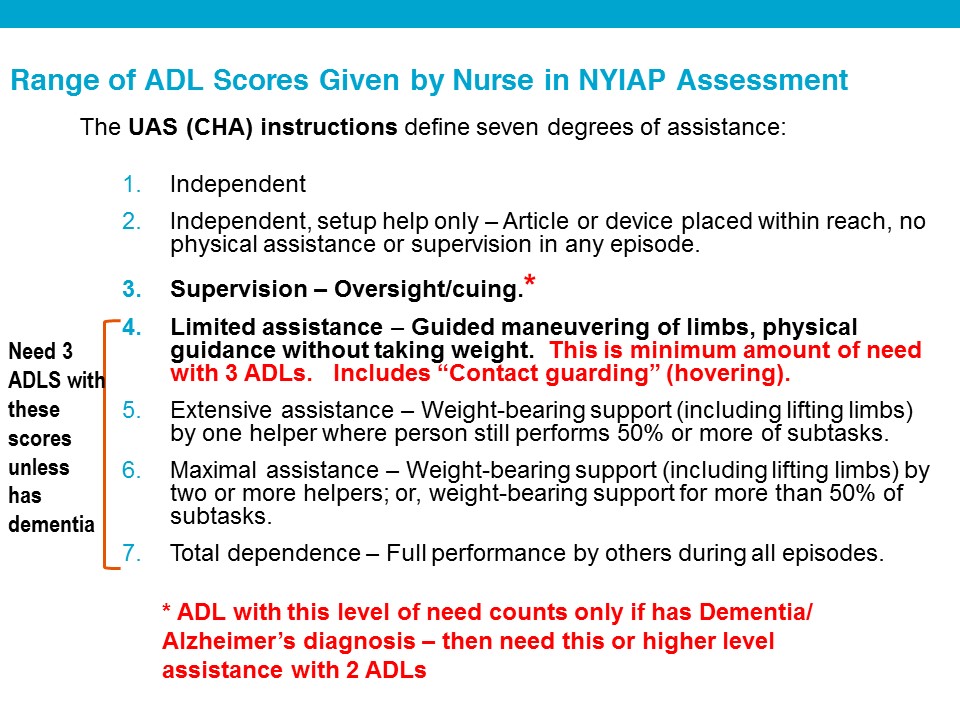
Eligibility for Personal Care and CDPAP services and enrollment in MLTC, for adults newly assessed for these services after Sept. 1, 2025, require the need for:
- "limited assistance with physical maneuvering" with THREE Activities of Daily Living (ADLs) or
- supervisory or oversight/cueing assistance with TWO ADLs for people diagnosed with Alzheimer's disease or dementia.
Two charts below show WHICH ADLs count toward the minimum thresholds, and the TYPE of ASSISTANCE that counts.
WARNING: 3-day "Lookback" Used To Assess ADL's � Nurse assessor is instructed to only record the person�s actual level of self-care and support actually received during the last 3 days before the assessment. This is according to the UAS-NY Reference Manual, Aug. 2022 edition pp. 28-33.
TIP: Consumer should have help with ADLs in at least one of the 3 days before the NYIAP nurse assessment. This can be informal help by a family member or paid help. Otherwise the ADLs will not count toward the minimum.
ALERT: The new ADL Thresholds ELIMINATE stand-alone Housekeeping �Level I� services now authorized by local districts up to 8 hours/week � a critical preventative service. This is because Housekeeping is a type of Personal Care for people who do not need assistance with ADLs but do need help with Instrumental ADLs (IADLs), and no one is eligible for Personal Care unless they have 3 ADLs. Those who received Housekeeping services before Sept. 1, 2025 will have Legacy Status (grandfathered in).
WHO - THE ADL THRESHOLDS ONLY APPLY TO ADULTS - NOT TO CHILDREN UNDER AGE 21
DOH revised its origianl June 2025 guidance documents in August 2025 to clarify that children under age 21 are NOT subject to the ADL thresholds for personal care or CDPAP. See revised guidance here.
In January 2026 - DOH isssued GIS 26 MA/02 - Legacy Status and Eligibility Criteria for Children Under 21 Seeking PCS/CDPAP Services (PDF) (Jan. 22, 2026) -Reiterates that the ADL thresholds do not apply to children under 21.
State DOH directives
Posted on the NYS DOH NY Independent Assessor Document Repository webpage)
-
25 OHIP/ADM - 03 (PDF) 6/30/25, Revised August 22, 2025: - New Minimum Needs Requirements for Personal Care Services (PCS) and Consumer Directed Personal Assistance Services (applies to local Depts. of Social Services (LDSS) that approve PCS and CDPAP for people who are exempt or excluded from MLTC or other Medicaid managed care plans.
-
Attachment Alzheimer's Disease or Dementia Form (DOH-5821) (PDF)
-
Revised in Aug. 2025 from the original issued June 30, 2025 to clarify the ADL thresholds do not apply to children under age 21
-
-
MLTC Policy 25.04: Minimum Needs Requirement Update to the Eligibility Requirements for Managed Long Term Care Enrollment - 6.30.2025 (applies to MLTC and MAP plans - but not PACE)
- Attachment Alzheimer's Disease or Dementia Form (DOH-5821) (PDF)
-
Directive to Medicaid Managed Care Plans, HIV Special Needs Plans (HIV SNPs), and Health and Recovery Plans (HARPs June 30, 2025, revised August 22, 2025 to clarify ADL thresholds do NOT apply to children under age 21.
-
GIS 26 MA/02 - Legacy Status and Eligibility Criteria for Children Under 21 Seeking PCS/CDPAP Services (PDF) (Jan. 22, 2026) Reiterates that the ADL thresholds (a/k/a Minimum Needs criteria) do not apply to children under 21.
-
UAS-NY Reference Manual, Aug. 2022 edition - Manual that instructs nurses on how to score ADLs and complete other parts of the Uniform Assessment Tool. Not publicly posted.
WHO IS GRANDFATHERED IN - who has "Legacy Status" -so does not need to meet the new Minimum ADL Criteria? And How can they KEEP Legacy Status?
-
GOOD NEWS - You did NOT need to be enrolled in an MLTC plan by Sept. 1, 2025 or be receiving Personal Care [PCS] or CDPAP from your managed care plan or local DSS/HRA by Sept. 1, 2025 in order to be grandfathered in.
-
For legacy status you must satisfy one of the four criteria below. You must be either --
-
Enrolled in MLTC plan as of 8/1/25 OR be authorized for PCS or CDPAP by the local DSS or mainstream managed care plan before Sept. 1, 2025, OR be
-
Assessed by NYIA on or after 9/1/2024 and before 9/1/2025 and enroll in MLTC or be authorized by DSS or a mainstream managed care plan for PCS/CDPAP within 1 year of the NYIAP assessment.
-
EXAMPLE: The NYIA assessment was in June 2025, but you did not enroll in MLTC until Nov. 1, 2025. You have legacy status and are NOT subject to the ADL thresholds as long as you enroll within one year of the June 2025 assessment. OR
-
-
NYIAP Assessment was scheduled before 9/1/2025, but was rescheduled to take place after 9/1/25. Appointment must be rescheduled through "no fault " of the consumer (no definition provided in directives) AND the rescheduling must have been done before the date of the initial scheduled appointment.
-
If ���Plan or Local DSS requests VARIANCE (a repeat assessment by NYIAP) � legacy status is given if the initial NYIAP assessment was done before 9/1/25, even if the re-assessment is conducted after 9/1/2025.
If you are grandfathered in (have legacy status) - how do you keep it? Can you lose it? TWO Types of Legacy Status:
-
Plan Legacy Status: If you are in an MLTC or MAP plan, you cannot have a break in being enrolled in some plan -- or you lose "Plan Legacy status." You may switch plans or switch to a different type of plan (MAP or PACE), but with no gap in enrollment. If you have a gap, you will lose Plan Legacy Status and may be subject to the new ADL thresholds.
-
Problems will arise if you are disenrolled from a plan for any reason and did not enroll in a new plan immediately. This can happen because you voluntarily disenroll - or if you are involuntarily disenrolled from a plan for reasons such as (see more in this article about involuntary disenrollment):
-
you were in a nursing home for more than 3 months (see here ),
-
or if you moved elsewhere in NYS and had to switch plans, or
-
you did not receive PCS/CDPAP or other community-based long term care services for the last month. MLTC members receiving CDPAP who did not switch to PPL, so have not received services for over a month, may be disenrolled from their plans. They risk being assessed under the new ADL standards if there is a gap in MLTC enrollment.
-
-
- "Service Legacy status" applies if you had PCS or CDPAP before 9/1/25 - whether from an MLTC plan, a mainstream managed care plan, or the local DSS/HRA. You keep Service Legacy status even if you have a gap in receiving those services after 9/1/25.
- If you are disenrolled from an MLTC plan, whether voluntarily or involuntarily, you should still have Service Legacy Status if you received PCS or CDPAP services from the MLTC plan before Sept. 1, 2025. If you want PCS/CDPAP later, after you are disenrolled from the MLTC plan, and if you fail the ADL TEST, you owill not be eligible to re-enroll in an MLTC plan. HOwever, you should be able to obtain PCS/CDPAP through the local DSS under the old standards. MLTC Policy 25.04 states, �Service Legacy is not impacted by an MLTC disenrollment and should not be changed.�
- How "service legacy" status works if one loses "plan legacy status" is unclear. Hopefully DOH will issue an FAQ to clarify how the consumer accesses PCS or CDPAP from their DSS,
- If you are disenrolled from an MLTC plan, whether voluntarily or involuntarily, you should still have Service Legacy Status if you received PCS or CDPAP services from the MLTC plan before Sept. 1, 2025. If you want PCS/CDPAP later, after you are disenrolled from the MLTC plan, and if you fail the ADL TEST, you owill not be eligible to re-enroll in an MLTC plan. HOwever, you should be able to obtain PCS/CDPAP through the local DSS under the old standards. MLTC Policy 25.04 states, �Service Legacy is not impacted by an MLTC disenrollment and should not be changed.�
How NYIAP uses the new ADL THRESHOLDS in the INITIAL "Independent Assessment" and how Consumer Shows they have Alzheimer's Disease or Dementia
If the consumer does not meet the 3-ADL criteria but has dementia or Alzheimer's Disease and needs supervisory assistance with 2 ADLs, their doctor or D.O. must sign a new Alzheimer's Disease or Dementia Form (DOH-5821) (PDF) and submit it to NYIAP. NYIAP is supposed to inform the consumer about the form when they call to schedule the assessment. The diagnosis must be made by a physician or D.O. - who need not be a NYS Medicaid provider.
-
It's unclear how consumer will submit the form to NYIAP if the assessment is by telehealth. DOH has said that the nurse will look at the form on the telehealth screen.
-
Reminder - be prepared to show that the Consumer needed help with the required 2 or 3 ADLs during the THREE days before the assessment. See more about the 3-day lookack here.
OUTCOME NOTICE from NYIAP with the Results of the Assessment -
The Outcome notice title is "Important Notice About Your Assessment Outcome." It is not called a "denial" or "approval" notice.
- If seeking to enroll in MLTC -- Outcome notice should say whether NYIAP finds they-
- ���Are Medically stable -- but note "MLTC plans should not deny enrollment for an individual determined medically unstable, unless the MLTC plan is unable to provide any other CBLTSS the individual is eligible to receive." MLTC Policy 25.04: Minimum Needs Requirement Update to the Eligibility Requirements for Managed Long Term Care Enrollment - 6.30.2025
-
whether they meet the new MInimum ADL critieria, and
-
whether they need assistance with community-based long term care for more than 120 days AND
-
If they do not have Medicare, or if age 18-21, notice must also say whether they were determined to need a "nursing facility level of care," meaning an "NFLOC" score of 5 on the NYIAP nurse assessment. NOTE that individuals age 18-21 are eligible for MLTC if they need nursing facility level of care, but do not have to pass the ADL Test.
-
If the NYIAP notice says:
-
medical condition is unstable, this is not a ground to deny MLTC enrollment, unless the MLTC determines that consumer is not eligible for other services, such as private duty nursing. MLTC Policy 25.04
-
that they do not need long-term care services for 120 days, but they do pass the ADL test, they may not enroll in MLTC or MAP, but should be able to request PCS/CDPAP from the local LDSS short-term. This is unclear.
-
-
Some notices tell the consumer she is not eligible for MLTC or a Medicaid Advantage Plus (MAP) plan but she may be eligible for PACE. See DOH info on PACE.
-
PACE is only for people age 55+ and is not available in every county. See this list of Partial, MAP, and PACE plans (scroll to the bottom for PACE)(Unclear if this list is updated).
-
Even if PACE is in client's county, it may not be conveniently located - or desirable. PACE, like Medicaid Advantage Plus, is a combined Medicare Advantage Plan with an MLTC plan. So.. if client has preferred doctors, she will not be able to see them with her Medicare coverage UNLESS they are in the PACE plan's network.
-
- If seeking PCS/CDPAP from a managed care plan or from local DSS, including Immediate Need, Outcome notice should say whether consumer:
- meets the new MInimum ADL critieria
-
is Medically stable (if not medically stable, not eliglble for PCS or CDPAP under state regulations)
NOTE: Outcome notices NYLAG has reviewed don't say whether client was determined to have DEMENTIA - which would mean just need 2 ADLs, or whether client failed to document she has dementia. Nor do notices say that client was determined to need limited assistance with 1 or 2 but not 3 ADLs, or identify which ADLs.
ADVOCACY & Requesting FAIR HEARINGS IF OUTCOME NOTICE DENIES MLTC enrollment or Services
-
Consider requesting a re-do reassessment by NYIAP - if NYIAP assessor overlooked the need for help with the required number of ADLs, if the consumer did not have a family member or other person present at the assessment to help point out their needs, or if telehealth was used which is not as effective as an in-person assessment. Also, if the client has dementia or Alzheimer's but did not document it, or if ADLs weren't identified because of the 3-day lookback rule.
-
REQUEST a copy of the assesments from NYIA to help evaluate what the initial assessment missed - by email NYIAPfairhearings@maximus.com or fax to 917-228-8899 - Submit a HIPPA if you are not the consumer. You do not have to wait until you request the Fair Hearing to request the assessments.
-
-
CONSUMER MAY REQUEST A FAIR HEARING iif Outcome Notice says not eligible for MLTC or for PCS/CDPAP from a mainstream Medicaid managed care plan or Local DSS.
-
Fair hearing is against the NY Independent Assessor Program (NYIAP) .
-
Request the hearing from the NYS OTDA Office of Administrative Hearings just like other Medicaid hearings.
-
You have 60 days to Request a Fair Hearing - starting with the date of the notice. You can ask that the hearing be expedited - see 22-03 Fair Hearings Transmittal Expedited Medicaid Hearings explains how to request and standards for expediting
-
REQUEST a copy of the assesments from NYIA if ELIGIBILITY DENIED - by email NYIAPfairhearings@maximus.com or fax to 917-228-8899 - \Submit a HIPPA if you are not the consumer. We do not believe you have to wait until you request the Fair Hearing to request the assessments.
-
Routine REASSESSMENTS after Sept. 1, 2025
All recipients of PCS or CDPAP must be reassessed every year - by their MLTC or mainstream plan or local DSS.
-
If consumer has Legacy Status, the plan or LDSS uses the old criteria - not the new ADL Thresholds.
-
If consumer does NOT have legacy status, plan or LDSS uses the new ADL thresholds.
-
If consumer does not meet the 3 ADL test, but has dementia or Alzheimer's and needs supervision with 2 ADLs, must submit a new Alzheimer's Disease or Dementia Form (DOH-5821) form even if submitted one before.
-
Guidance does not state what notice and procedures must be followed if a Plan or LDSS decide consumer who does NOT have legacy status does not meet the new ADL thresholds. Presumably an advance 10-day written notice of discontinuance must be issued with appeal rights.
-
If in a managed care plan, this would be an Initial Adverse Determination with the right to request a plan appeal. See more about managed care appeal rights here.
-
If in DSS, this would be a Notice of Discontinuance or change with Fair Hearing rights.
-
-
Either way, consumer is entitled to AID CONTINUING if they request the appeal before the effective date (or, if requested before 12/31/25, before the statute of limitations expires for the appeal).
CMS approval of the ADL thresholds - and NYS Senate Bill to Repeal them
CMS approved these new restrictions in a 10/31/24 letter closing out -- approving - the state�s request to amend the 1115 waiver to apply the ADL restrictions to eligibilty for MLTC enrollment. NOTE that Tte CMS letter states in part:
- "New York has an independent and separate obligation under federal laws including, but not limited to, the Americans with Disabilities Act, Section 504 of the Rehabilitation Act, Section 1557 of the Affordable Care Act, or the Supreme Court�s Olmstead decision to ensure that individuals are served in the most integrated setting appropriate to their needs.... However, as we note, New York has an obligation to ensure eligibility standards do not discriminate based on disability under CMS and other federal nondiscrimination regulations."
NYLAG supports Senate BIll S358 (Gustavo Rivera)/A1198(Amy Paulin) (2025-26) that would repeal the ADL thresholds, which advocates contend discriminates against people with various disabilitiies who will be denied services. Download NYLAG's memos in support of the bill repealing the lookback here and the ADL restrictions here.