|
|
NYS Medicaid Redesign Team II (MRT) - Minimum 3-ADL Thresholds START Sept. 1, 2025 for New Home Care and MLTC Enrollees
02 Jul, 2025
This article gives updates on the Medicaid changes enacted in the 2020 NYS Budget under the "Medicaid Redesign Team II" or MRT-2. These are the:
-
Three-ADL Minimum Threshold to qualify for Personal Care and CDPAP and enroll in MLTC - will start Sept. 1, 2025 - see more here.
- The Maintenance of Effort requirements that banned the State from implementing these restrictions -- which may be over.
-
30-month Lookback (Not yet in effect - per ARPA Maintenance of EFfort)
-
The New York Independent Assessor Program (NYIAP) is already in effect see this article.
-
Diminishing Transition Rights for People Required to Change or Enroll in an MLTC plan - See this article and FACT SHEET about the amended regulation effective Nov. 8, 2021.
-
Other Changes in Medicaid Home Care Enacted in 2020
This change in eligibility was enacted in 2020 but has been on hold ever since because of Maintenance of Effort Requirements under the federal ARPA COVID relief law- see more here.
What are the New Minimum ADL Thresholds?
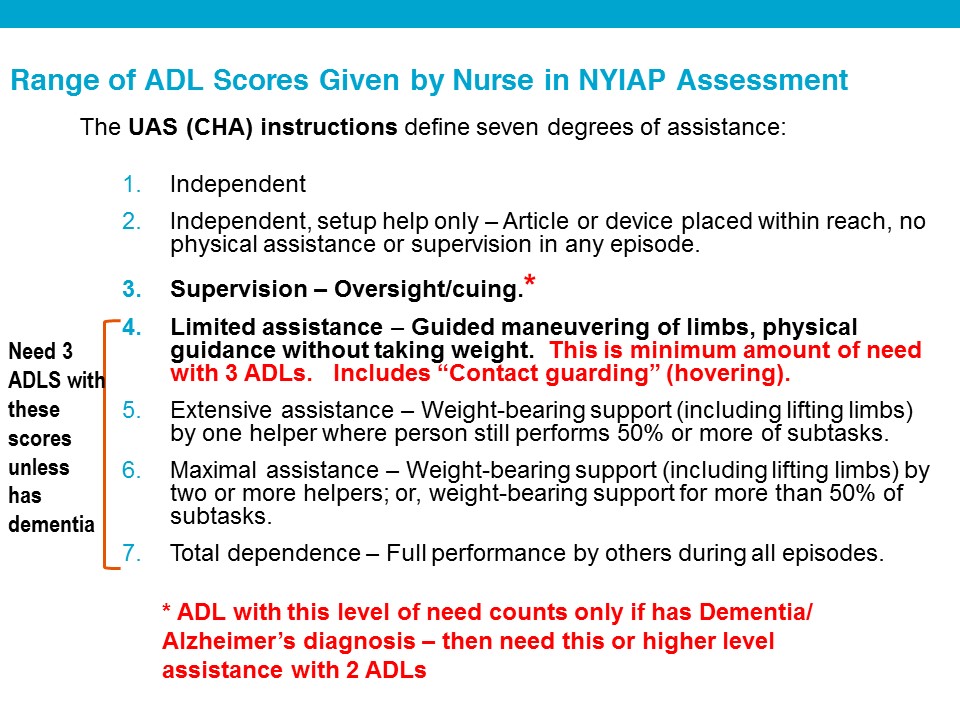
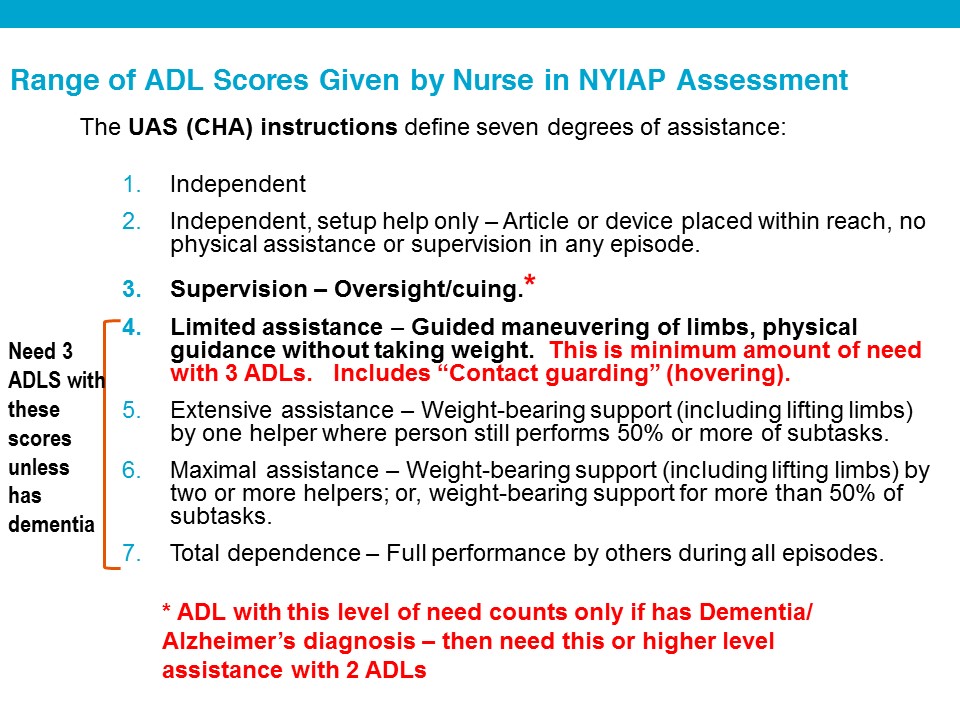
Eligibility for Personal care and CDPAP services and enrollment in MLTC will, after Sept. 1, 2025, require the need for "limited" assistance with physical maneuvering" for THREE Activities of Daily Living (ADLs) or supervisory assistance with TWO ADLs for people diagnosed with Alzheimer's disease or dementia.
- ALERT: This will ELIMINATE stand-alone Housekeeping “Level I” services now authorized by local districts up to 8 hours/week – a critical preventative service.
On June 30, 2025, State DOH posted two directives announcing that these eligibility restrictions will start Sept. 1, 2025:
-
25 OHIP/ADM - 03 - New Minimum Needs Requirements for Personal Care Services (PCS) and Consumer Directed Personal Assistance Services
-
MLTC Policy 25.04: Minimum Needs Requirement Update to the Eligibility Requirements for Managed Long Term Care Enrollment - 6.30.2025
-
GOOD NEWS - You do NOT need to be enrolled in an MLTC plan by Sept. 1, 2025 or receiving Personal Care [PCS] or CDPAP from your managed care plan or local DSS/HRA by Sept. 1, 2025. But you must be ASSESSED BY NYIAP between Sept. 1, 2024 and Sept. 1, 2025 -- and enroll in an MLTC Plan or be authorized for PCS/CDPAP by your local DSS WITHIN ONE YEAR of hat assessment. See below for detailed requirements for legacy status.
-
TIP: Get assessed by NYIAP before Sept. 1, 2025!
Here are the detailed criteria for "Legacy Status" in the above directives. For legacy status you must be EITHER:
-
Enrolled in MLTC plan as of 8/1/25 OR assessed and authorized by the local DSS for PCS or CDPAP before Sept. 1, 2025, OR you must be
-
Assessed by NYIA on or after 9/1/2024 and before 9/1/2025 but not yet enrolled in MLTC or not yet authorized by the local DSS for PCS/CDPAP before 9/1/2025 – as long as you enroll in MLTC or are authorized by DSS for PCS/CDPAP within 1 year of the NYIAP assessment.
-
EXAMPLE: The NYIA assessment was in June 2025, but you do not enroll in MLTC until Nov. 1, 2025. You have legacy status and are NOT subject to the ADL thresholds as long as you enroll within one year of the June 2025 assessment. OR
-
NYIAP Assessment scheduled before 9/1/2025, but was rescheduled to take place after 9/1/25. Appointment must be rescheduled through "no fault " of the consumer (no definition provided in directives) AND the rescheduling must have been done before the date of the initial scheduled appointment.
-
Plan or Local DSS requests VARIANCE (a repeat assessment by NYIAP) – legacy status given if the initial NYIAP assessment was done before 9/1/25, even if the re-assessment is conducted after 9/1/2025.
If you are grandfathered in (have legacy status) - how do you keep it? Can you lose it?
-
If you are in an MLTC plan, you cannot have a break in enrollment or you lose "Plan Legacy status." You may switch plans or switch to a different type of plan (MAP or PACE), but with no gap in enrollment. If you have a gap, you will be subject to the new ADL thresholds.
- "Service Legacy" status is different than Plan legacy. If you had PCS/CDPAP before 9/1/25 and are disenrolled from an MLTC plan, you may still qualify for PCS/CDPAP under the old standards. The MLTC Policy directive states, “Service Legacy is not impacted by an MLTC disenrollment and should not be changed.” The exact meaning of this is unclear - presumably the individual could enroll in the NHTD waiver and receive PCS/CDPAP if they otherwise have "legacy status" for these services.
-
If the consumer may not meet the 3-ADL criteria but has dementia or Alzheimer's Disease and needs supervisory assistance with 2 ADLs, their doctor or D.O. must sign a new Alzheimer's Disease or Dementia Form (DOH-5821) and submit it to NYIAP. The form is not yet posted online. NYIAP is supposed to inform the consumer about the form and provide it. The diagnosis must be made by a physician or D.O. - who need not be a NYS Medicaid provider. (It's unclear how consumer will submit the form to NYIAP if the assessment is by telehealth).
-
OUTCOME NOTICE from NYIAP -
-
If seeking to enroll in MLTC.
-
Outcome notice should say whether NYIAP finds they-
-
need assistance with community-based long term care for more than 120 days AND
-
starting Sept. 1, 2025 - whether they meet the new MInimum ADL critieria - need for "limited" assistance with physical maneuvering" for THREE Activities of Daily Living (ADLs) or supervisory assistance with TWO ADLs for people diagnosed with Alzheimer's disease or dementia.
-
Are Medically stable -- but note "MLTC plans should not deny enrollment for an individual determined medically unstable, unless the MLTC plan is unable to provide any other CBLTSS the individual is eligible to receive." MLTC Policy 25.04: Minimum Needs Requirement Update to the Eligibility Requirements for Managed Long Term Care Enrollment - 6.30.2025
-
If do not have Medicare, or if age 18-21, must also need a "nursing home level of care," meaning a score of 5 on the NYIAP CHA assessment.
-
If Outcome Notice says not eligible for MLTC, consumer may request a Fair Hearing . Unclear if the Outcome Notice will specify WHICH criteria are not met for MLTC - the 3 ADL standards or not needing any services for 120+ days. If the notice says medical condition is unstable, however, MLTC may not deny enrollment unless they determine that consumer is not eligible for other services, such as private duty nursing. MLTC Policy 25.04
-
If Outcome notice finds NOT eligible for MLTC, if the reason is they fail the new ADL TEST, if the NYIAP assessment was done after 9/1/25, they may NOT request Housekeeping services of 8 hours/week from the local DSS. If the reason is they do not need long-term care services for 120 days, they should be able to request PCS/CDPAP from the local LDSS short-term.. This is unclear.
-
If seeking PCS/CDPAP from a managed care plan or from local DSS, including Immediate Need, Outcome notice should say whether:
-
Starting Sept. 1, 2025 - whether they meet the new MInimum ADL critieria - need for "limited" assistance with physical maneuvering" for THREE Activities of Daily Living (ADLs) or supervisory assistance with TWO ADLs for people diagnosed with Alzheimer's disease or dementia.
-
Are Medically stable
- If Outcome Notice says not eligible for PCS/CDPAP consumer may request a Fair Hearing . Unclear if the Outcome Notice will specify WHICH criteria are not met f- the 3 ADL standards or not medically stable - or both.
-
IF consumer has Legacy Status, plan or LDSS uses the old criteria - not the new ADL Thresholds.
-
If consumer does NOT have legacy status, plan or LDSS uses the new ADL thresholds.
-
If do not meet the 3 ADL test, but consumer has dementia or Alzheimer's and need supervision with 2 ADLs, must submit a new form even if submitted one before.
-
Guidance does not state what notice and procedures must be followed if a Plan or LDSS decide consumer who does NOT have legacy status does not meet the new ADL thresholds. We hope to confirm with DOH:
-
If receiving PCS or CDPAP from a mainstream managed care plan or Local DSS/HRA, an advancee written notice of discontinuance msut be issued with appeal rights. If in a managed care plan, this would be an Initial Adverse Determination with the right to request a plan appeal. See more about managed care appeal rights here. If in DSS, this would be a Notice of Discontinuance or change with Fair Hearing rights. Either way, consumer is entitled to AID CONTINUING if they request the appeal before the effective date (or, if requested before 12/31/25, before the statute of limitations expires for the appeal).
CMS approved these new restrictions in a 10/31/24 letter closing out -- approving - the state’s request to amend the 1115 waiver to apply the ADL restrictions to eligibilty for MLTC enrollment. NOTE that Tte CMS letter states in part:
- "New York has an independent and separate obligation under federal laws including, but not limited to, the Americans with Disabilities Act, Section 504 of the Rehabilitation Act, Section 1557 of the Affordable Care Act, or the Supreme Court’s Olmstead decision to ensure that individuals are served in the most integrated setting appropriate to their needs.... However, as we note, New York has an obligation to ensure eligibility standards do not discriminate based on disability under CMS and other federal nondiscrimination regulations."
NYLAG supports Senate BIll S358 (Gustavo Rivera)/A1198(Amy Paulin) (2025-26) that would repeal the ADL thresholds, which advocates contend discriminates against people with various disabilitiies who will be denied services. Download NYLAG's memos in support of the bill repealing the lookback here and the ADL restrictions here.
Neither the 30-month lookback or the 3-ADL eligibility restriction can start until CMS certifies that the state has spent federal funds under the American Rescue Plan (ARPA). The ARPA law has a Maintenance of Effort Requirement that says states cannot restrict eligibility for home and community based services (HCBS) until the earlier of when they spend the federal ARPA funds or March 31, 2025. See this link. See NYS ARPA website for its spending plan and quarterly reports to CMS.
CMS must issue a "close out" letter finding that the ARPA funds have been spent, posted on this CMS website. However, we learned on July 2, 2025 that CMS did issue this letter to NYS but that it is not posted. This means that both the ADL Restrictions and the 30-month Lookback may be implemented. (However see below re other steps needed before Lookback is implemented.
|
LOOKBACK - DOH has informally stated that the earliest date for implementation is in 2025 - though the date on NYS MRT 2 webpage is still March 31, 2024. Given the approvals still outstanding from CMS, and the lack of any DOH procedures instructing the local Medicaid offices about the lookback, it seems unlikely it can start until at least ater in 2025.
NYLAG supports a bill A1907 - S04786 that would REPEAL the 30-month lookback. Download memo in support here (2025-26)
The lookback cannot begin until the following happen, which have not happened as of July 2, 2025:
-
The federal Medicaid agency - CMS - approves NYS's spending of American Rescue Plan (ARPA) funds . See more here about ARPA and how to track when CMS says the ARPA restriction is over . However, as the State is moving ahead to implement the ADL thresholds, it seems that CMS may have approved the ARPA spending.
-
CMS approves a State Plan Amendment of the Medicaid plan
-
CMS approves DOH's request to amend the 1115 waiver to allow a lookback to be used to limit eligibility for MLTC enrollment. DOH filed this request in March 2021, which was amended in August or September 2022.
-
On May 5, 2021, NYLAG submitted comments on the State's March 2021 proposal to CMS to amend the 1115 waiver to allow the lookback to apply to MLTC enrollment (PDF). CMS "Completeness letter" dated April 7, 2021 - (Web) - (PDF). Earlier, NYLAG posted COMMENTS to the State's preliminary proposal to amend the 1115 waiver to apply the LOOKBACK to MLTC enrollment.
-
CMS "Completeness letter" dated April 7, 2021 - (Web) - (PDF).
-
Earlier, NYLAG posted COMMENTS to the State's preliminary proposal to amend the 1115 waiver to apply the LOOKBACK to MLTC enrollment.
-
Track updates on this request on the CMS 1115 Waiver update page.
-
DOH develops and issues directives to the local Medicaid agencies with policies, procedures and forms to implement the lookback. These have not been issued as of Feb. 25, 2025.
Once the lookback goes into effect, applications filed for Medicaid in order to obtain any community-based long term care service will have a “lookback” of 30 months (2.5 years). Applications filed before the effective date -- whatever it is -- will have no lookback. So for those applications, transfers of assets after Oct. 1, 2020 will not trigger any transfer penalty. Check back to this website for news to see if this extension is confirmed.
HOW LONG IS THE LOOKBACK? The lookback will require records back 30 months before the application. When it was first enacted in 2020, the lookback would have been phased in, starting with shorter periods and then eventually being 30 months. It is unclear if it will be phased in when finally implemented, or if it will be 30 months from the beginning.
Both Applicant and spouse must submit all financial records during the lookback period, even if the spouse is not applying for Medicaid or is doing a spousal refusal.
Transfers made during the lookback period could trigger a transfer penalty unless they are exempt transfers. The length of the penalty will be calculated the same as it is for nursing homes. In NYC home care would be denied for one month for every $13,037 transferred (2021 - see GIS 20 MA/12). See penalty rate in the rest of the state in GIS 20 MA/12 (2021) (Sec. 13, 14) See the PowerPoint for more information
|
|
-
Which services does the lookback apply to? The law specifies home health care services, private duty nursing services, personal care services (which likely include CDPAP), and assisted living program services. DOH may designate others by regulation. Since MLTC plans deliver these services, presumably the lookback will apply to MLTC enrollment.
-
The usual exceptions would apply–transfers to the spouse, transfers by an individual under 65 to a supplemental needs trust, transfer to a disabled child. See exceptions to the transfer penalty for a nursing home here. Since the home is exempt while an individual is living in it, subject to the home equity limit, it is our hope that a penalty may not be imposed on the transfer of a home - but DOH's March 2021 proposal to CMS says transfers of the home would be subject to the same penalties with the same exceptions that apply for nursing home care. Advocates disagree. Many policies like this will be fleshed out later.
-
The lookback will inevitably cause long delays in processing applications, not to mention compiling the documents needed to apply. It is our view that the Medicaid agencies must comply with the time limits for approvals – generally 45 days, and 90 days if a disability determination is required, and faster for Immediate Need cases. Yet even now, applications often exceed these limits, and this will add more work for the local districts. There are many questions about implementation – this is just the bare bones as we understand it now.
-
TIP: Medicaid applications filed now should request coverage of CB-LTC, in order for the consumer to be "grandfathered in" with no lookback required later, after the lookback goes into effect. In order to request coverage of CB-LTC, be sure to include Supplement A DOH 5178A with the application (which must now be included with all Medicaid applications anyway - see this article). Links to the statewide Supplement A Form DOH-5178A are in this article, which explains that NYC no longer uses a different form).
-
TIP: On the Supplement A DOH 5178A form (link here), Question 8 on page 3 asks you to check one of THREE boxes to indicate the type of care and services applicant is seeking. The 1st two choices are both for Community-Based coverage. Choose the SECOND box seeking community Medicaid with Community-Based Long Term Care, to improve chances that the application will be grandfathered in. NOTE that final policies on exactly which individuals have been grandfathered in have not been issued, but DOH's final submission to CMS requesting amendment of the 1115 waiver governing the MLTC program says that those "who apply for Medicaid coverage of CBLTC before the implementation date will not be subject to the 30-month lookback, including those individuals who file a pre-implementation date application for Medicaid coverage of CBLTC but who are not yet receiving CBLTC services under that application on the implementation date." Final version submitted to CMS March 25, 2021 (Web) - (PDF at page 6).
|
|
-
DOH is scaling back usage of MLTC plans that are “partially capitated”–meaning that Medicare services are not included. They will be expanding “fully capitated” plans – which are Medicaid Advantage Plus and PACE. There will be expanding “fully capitated” plans – which are Medicaid Advantage Plus and PACE. The FIDA program was fully capitated but it closed last year. (sec 5) Read about types of plans here.
-
DOH is setting a cap on enrollment by individual MLTC plans, in an effort to limit the rapid growth in certain plans, which may result from aggressive marketing by the plan and its contractors. The penalty for exceeding the cap will be withholding of up to 3 percent of the premium.
SIDE NOTE – NYLAG fears that plans will control their enrollment by excluding the high-need consumers while welcoming those with lower needs(sec. 5).
-
Instead of a nurse assessment twice a year, MLTCs will now assess once a year unless there is a need for an additional assessment. (sec. 22). The assessments are by NY Medicaid Choice.
-
Transportation will be carved out of MLTC service package–DOH will contract with a transportation broker. (Part LL, sec. 2)
-
Mandatory Auto-Enrollment of dual eligibles enrolled in Medicare Dual Eligible Special Needs Plan (Dual-SNP) into Medicaid Advantage plans when they turn 65, or into Medicaid Advantage Plus (MAP) plans if they receive home care. This is part of the push to the “full capitation” mega-plans that cover both Medicaid and Medicare. Initially, this will primarily affect people who had MAGI Medicaid under age 65, then are transitioned to non-MAGI Medicaid at 65. Most were in mainstream Medicaid managed care plans, so they will be transferred to the “sister” Medicaid Advantage Plan of the same company. (Sec. 6) (Medicaid Advantage is like Medicaid Advantage Plus except these plans do not provide any Medicaid long-term care services. Only MAP plans provide Medicaid long-term care services).
-
New applicants for Medicaid seeking home care will no longer be informed of the availability of CDPAP. (sec 17).
-
Various limits on CDPAP access, such as new people approved for Medicaid will no longer be informed of the availability of CDPAP services.
-
2020 Budget required DOH to procure a new standardized task-based assessment tool, about which advocates have raised concerns. This was never implemented and Gov. Hochul's proposed Budget for 2022-23 abandoned this effort and instead just issued guidelines and standards for plans and local districts to make appropriate and indivdiualized determinations for utilization. A uniform "tasking tool" that would presumably translate findings made in the Uniform Assessment System nurse assessment (a/k/a Community Health Assessment) into a plan of care with the number of hours to be approved. The law says the tool must be “ evidence-based” and used “to assist managed care plans and local departments of social services to make appropriate and individualized determinations for ... the number of personal care services and CDPAP hours of care each day.“ The tool is supposed to identify how Medicaid recipients' needs for assistance with activities of daily living can be met through telehealth and family and social supports. (Section 21). In early May 2021, DOH posted a Request for Information for the new Uniform Tasking Tool.
Click here to download NYLAG's position paper that opposed the cuts and
Read about real people who would be hurt by each of these cuts.
Click here to download the executive summary of the Medicaid Redesign Team (MRT) II proposals.
See also Medicaid Matters NY coalition statements on the NYS Budget and MRT II.
|