By The Legal Aid Society This guide will answer common questions about how to use your Medicaid to get health care services. It will cover:
Understanding Your Medicaid PlanDo I have Medicaid through “fee-for-service” or through a “managed care plan”?To start the process of getting health care services using your Medicaid, the first thing you should know is whether you get your Medicaid directly through the city or state, called “fee-for-service Medicaid” or “straight Medicaid,” or if you get your Medicaid through a private health insurance plan, called a “Medicaid managed care plan.” You can figure this out by:
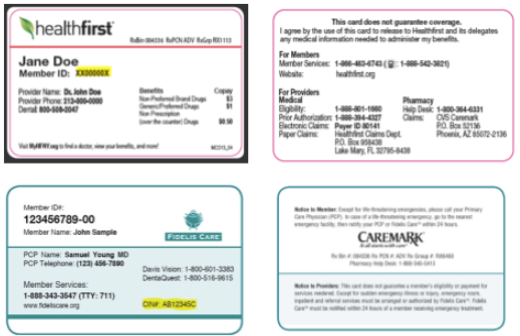
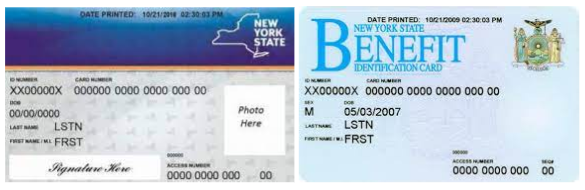
If the only Medicaid card you use is a New York State benefits card, you probably have fee-for-service or straight Medicaid. You should have a card that looks like one of the cards below even if you also have a plan card. NOTE: If you also receive cash assistance and/or SNAP (also known as food stamps), you use this card for those benefits as well.
I get my Medicaid through a “Medicaid managed care plan.” What is that and how does it work?A Medicaid managed care plan is a private health insurance plan that works with a group of doctors, clinics, hospitals and pharmacies to provide your care. This is called a “network.” You can only see these “in-network” doctors. You will need to choose one of the doctors from the health plan to be your primary care provider (PCP). Your PCP will provide most of your care. You may need a referral from your PCP to see a specialist and for other services. What health care services are covered by Medicaid?Whether you get your Medicaid through a managed care plan or fee-for-service, Medicaid pays for all medically necessary covered services, including:
Can I be charged for health care services that are covered by Medicaid?If you go to a provider that takes your Medicaid, you can only be charged limited co-payments for health care services that are covered by Medicaid. Some of these co-payments include:
A provider can send you a bill for any unpaid amount, but a provider cannot refuse to give you a health care service if you cannot pay the co-payment, or if you have an outstanding balance from a prior visit. Finding a DoctorIf I need to find a primary care provider, dentist, or other health care provider that takes my Medicaid, what do I do?There are several ways you can find a health care provider in your area that takes your Medicaid plan:
Always call the doctor before making an appointment to confirm that they accept your Medicaid. My Medicaid managed care plan said I need to choose a primary care provider, how do I do that?If your Medicaid managed care plan says that you need to choose a primary care provider (PCP) and you already have an in-network provider that you want to be your main provider, all you have to do is call your plan and give them the name and contact information for that provider. If you need to find a provider that you want to be your PCP, follow the steps above to find an in-network provider, call the provider’s office to make sure that they are taking new patients, and then call your plan and give them the name and contact information for that provider as your new PCP. You can change your PCP at any time by calling your plan and giving them the name and information for your new provider of choice. Remember, you must always chose an in-network provider. If you do not choose your own PCP, your plan may assign you one. Getting CareI have a doctor or specialist that takes my Medicaid, what do I do to get the care I need from them?Make an appointment with your doctor. Be sure to bring your Medicaid card(s) and any other insurance cards you have with you to the appointment and give them to the office receptionist before your visit. Bringing all your insurance cards with you and giving them to the office before every visit helps protect you from being accidentally billed. If you doctor decides that you need a health care service, like a surgery, prescription drug, or dental filling, Medicaid may agree to pay for the service without any delay or extra paperwork. But some services require prior authorization, also called prior approval, before Medicaid will agree to pay for them. What is prior authorization?Some health care services are covered by Medicaid, but only if your provider proves that you meet certain criteria. This is called prior authorization, also called prior approval. If a health care service requires prior authorization, your provider has to get permission from your Medicaid managed care plan or Medicaid fee-for-service before giving you the care or medication you need. If your provider does not get this permission, Medicaid may not pay for it. The Medicaid-covered services that require prior authorization are listed in your Medicaid managed care Member Handbook. If your provider is telling you that a service is not covered or requires prior authorization, you can also call your plan and ask. If a health care service requires prior authorization, your managed care plan, or the State Department of Health if you have fee-for-service, will have criteria or standards that you must show you meet in order for you get the health care service from Medicaid. For example, your plan may only cover a more expensive brand name drug if your doctor can show why a less expensive generic drug does not work as well for you. Often, doctors are required to prove that the service you need is “medically necessary” for you. This means that your doctor needs to show how the service is necessary to treat your medical condition that is causing you problems. For example, Medicaid will only “authorize” and pay for home care services for you if a doctor can show that you cannot do activities of daily living on your own. If a service that you need requires prior authorization, your provider should ask your plan or fee-for-service Medicaid what criteria you need to meet to get approval for the service. Then your provider should submit a prior authorization request to the plan or Medicaid fee-for-service explaining why and how you meet those standards. Your doctor should include any medical documentation and records that help prove this point. If a delay in receiving the requested service would seriously harm your life or health, your provider should note this and ask for “expedited review”. How long does Medicaid have to make a decision on a prior authorization request?After your provider submits a prior authorization request, Medicaid must make a decision within three business days of receiving all necessary information. If your provider asked for and your Medicaid granted expedited review, Medicaid must make a decision within 72 hours of receiving the request. Medicaid can extend these deadlines to up to 14 calendar days if more information was needed from you or your provider to make a decision. What notice will I get if Medicaid approves my service?If Medicaid approves your request, you will receive written notice of the approval in the mail. Your provider will also receive notice of the approval. Depending on how your provider receives notices, they may receive it in the mail or electronically. Appealing a DenialWhat notice will I get if my Medicaid denies my service?
How do I appeal my Medicaid managed care plan’s decision to deny my service?Plan Appeal If you want to appeal your Medicaid managed care plan’s decision to deny your service, you first have to file an appeal with your plan called a Plan Appeal, also sometimes called an internal appeal. You have 60 days from the date on the Initial Adverse Determination notice to request a Plan Appeal. Instructions on how to request the Plan Appeal are included on the Initial Adverse Determination notice.
If your need is urgent, you can ask for a “fast-tracked” appeal. Your plan has to make a decision within 30 days of receiving your appeal request. If you asked for the appeal to be fast-tracked, your plan must make a decision within 72 hours. What if I lose my Plan Appeal? If you lose your Plan Appeal, you will receive a written denial notice in the mail called a “Final Adverse Determination.” This notice will explain why the plan denied your care and give you a deadline and instructions for appealing the denial. You have two options to appeal the Final Adverse Determination, a Fair Hearing or an External Appeal.
How do I appeal a Medicaid fee-for-service decision to deny my service?If you have Medicaid fee-for-service and Medicaid has denied your service, your only option to appeal the denial is to request a Fair Hearing. You have 60 days from the date on the denial notice to request a Fair Hearing. At a Fair Hearing, an Administrative Law Judge will review Medicaid’s decision and your evidence to determine whether you and your provider have proven that you meet the prior authorization standards for the service you need. A decision by the Administrative Law Judge is final and overrules any decisions by Medicaid. For more on how to request a Fair Hearing and the Fair hearing process, go to this Know Your Rights document here. DisclaimerThe information in this document has been prepared by The Legal Aid Society for informational purposes only and is not legal advice. This information is not intended to create, and receipt of it does not constitute, an attorney-client relationship. You should not act upon any information without retaining professional legal counsel.
|