By the Legal Aid Society This guide will answer common questions about New York State’s new Medicaid pharmacy benefits program, NYRx, which took effect April 1st, 2023. How does NYRx work?Through NYRx, New York State Medicaid will now pay for your drugs and medical supplies when you are at the pharmacy. Your health plan will no longer be paying for these benefits. Am I affected by this pharmacy benefit transition?If you are currently enrolled in a Mainstream Medicaid Managed Care Plan, a Health and Recovery Plan (HARP), or an HIV Special Needs Plan (HIV-SNP), you are automatically enrolled in NYRx. If you are enrolled in a Managed Long-Term Care Plan (MLTC), Medicaid Advantage Plus (MAP), Program of All-Inclusive Care for the Elderly (PACE), an Essential Plan (EP), or Child Health Plus (CHP), then NYRx does not apply to you. What does the NYRx pharmacy benefit include/cover?NYRx will cover the following:
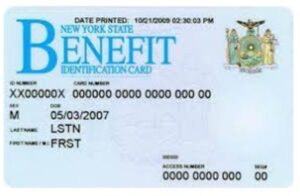
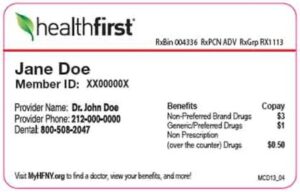
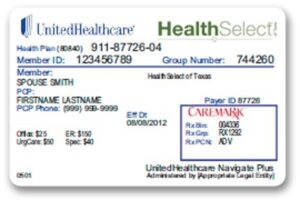
Does NYRx honor my existing Prior Authorizations or Approvals (PAs)?Yes. PAs issued by Medicaid Managed Care plans prior to April 1, 2023 (that are active/valid after April 1, 2023) will be honored and transferred to NYRx. If there is an issue at the pharmacy for a drug or supply that has already been approved, ask the pharmacist to call the Magellan call center at 877-309-9493 Can I get a prescription or supply fill without a Prior Authorization (PA)?Yes. From April 1, 2023, through June 30, 2023 you may receive a one-time, temporary fill for up to a 30-day supply of a drug that would normally require PA under NYRx. If there is an issue at the pharmacy with obtaining the fill, you should ask the pharmacist to call the Magellan call center at 877-309-9493. After receiving a one-time temporary fill for a non-preferred drug or supply, you must talk to your prescribing doctor or pharmacist about either submitting a request for PA to NYRx or switching to an alternate drug or supply that does not require PA. What happens if my Prior Authorization or Approval (PA) is denied under NYRx?Under NYRx your doctor (the prescriber) has the final say with respect to PAs. For example, if your doctor determines that use of a prescription drug is warranted, your doctor’s determination is final. This applies for every drug category; however your doctor will still be required to provide NYRx with the information and/or clinical documentation required for PA requests. Is it possible to receive an emergency fill or refill without prior authorization?If you have a valid prescription, pharmacists may provide up to a 3-day emergency supply of medication by completing the emergency authorization process. You may tell the pharmacist to call the Magellan call center 877-309 9493 for assistance. How do I know if my pharmacy is participating in NYRx?Most pharmacies in New York State participate in NYRx. You can locate NYRx-participating pharmacies here. If your pharmacy does not take Medicaid, you may ask your doctor to send a new prescription or transfer a refill to a pharmacy that participates in NYRx. Do I need a new pharmacy benefits card?No. To obtain medication, you may present your Common Benefit Identification Card (CBIC), also known as your New York State (NYS) Benefits Identification Card. You may also show your Medicaid health plan card. Both cards have your CIN (client identification number), which the pharmacist will use to bill NYRx for your drugs and/or supplies.
Health plan cards look like this:
Will my co-payments for OTC drugs, prescriptions, or DME change?No, your co-payments will not change. All co-payments will stay the same:
What if I am in the Restricted Recipient Program (RRP)?If you were a member of the RRP prior to April 1, 2023, you will remain restricted for services under NYRx. RRP members will continue to coordinate changes on their restrictions as they relate to pharmacy benefits through the New York City Human Resources Administration (HRA) Recipient Restriction (RR) unit. Changes related to your restriction to a pharmacy, if appropriate, will be processed by the HRA RR staff. Get HelpFor more information, you may call the NYRx Medicaid Helpline at 855-648-1909 (800-662-1220 TTY), Mon – Fri 8 am – 8 pm and Sat 9 am – 1 pm or email NYRx@health.ny.gov. If you require legal assistance with your individual case, you may call The Legal Aid Society’s Access to Benefits helpline at 888-663-6880. DisclaimerThe information in this document has been prepared by The Legal Aid Society for informational purposes only and is not legal advice. This information is not intended to create, and receipt of it does not constitute, an attorney-client relationship. You should not act upon any information without retaining professional legal counsel.
|